The Greatest Epidemics in History: Epidemic Chronology.
Some of the Greatest Epidemics in History have been detected with archaeological findings on a wide historical scale from ancient times to the present day, and some have been recorded with historical inscriptions and transferred to the present day. Although some of them remain completely mysterious even today, with developing medical and technological opportunities, we can get to know these diseases more closely and identify their strengths and weaknesses in the laboratory environment. Let’s now take a look at the Greatest Epidemics in History that have left and continue to leave their mark on world history.
-
The Greatest Epidemics in History (China Circa 3000 BC)
About 5,000 years ago, an epidemic in China wiped out a village. The bodies of the dead were stuffed into a house and burned. Since the skeletons of young people and middle-aged people were found in the same place in the house, an average age could not be determined due to the skeletons mixing together. The archaeological site is now called “Hamin Mangha” and is one of the best-preserved prehistoric sites in northeastern China. Archaeological and anthropological findings indicate that the epidemic occurred quickly and that there was not enough time for proper burial and the area was not resettled.
Before the discovery of Hamin Mangha, another prehistoric mass grave dating to roughly the same period was found in a site called Miaozigou in northeastern China. These discoveries show that it spread to different regions and ravaged more than one region.
- The Greatest Epidemics in History Plague of Athens (430 BC)
Around 430 BC, shortly after the war between Athens and Sparta began, a disease broke out that would ravage the people of Athens and last for 5 years. According to some estimates, the death toll has risen to 100,000. Greek historian Thucydides (460-400 BC) wrote: “Even people in good health suddenly experienced severe fever in their heads, redness and inflammation in their eyes, throat and the inside of their mouths such as the tongue. It caused bloody and unnatural vomiting. “(Source: Translated from Richard Crawley’s book “The History of the Peloponnesian War”. London Dent, 1914).
What exactly this epidemic is from a biological perspective has long been a source of debate among scientists. Considering the symptoms from the findings, a number of disease possibilities were considered, including Typhoid fever and Ebola. Many scientists believe that overcrowding caused by the war worsened the epidemic. During the ongoing war between Sparta and Athens at that time, the Spartans, who were stronger on land, forced the Athenians to take shelter behind the city walls. The epidemic spread rapidly among the people of Athens, who were trapped under siege within the walls. This war continued until 404 BC, when Athens was forced to surrender to Sparta, despite the ongoing epidemic. It is known that Pericles, the great leader of Athens, also died in this epidemic.
When the soldiers returned from the campaign to the Roman Empire, they brought back with them more than just the spoils of victory. It has been written that the Antonine Plague, a disease of smallpox, devastated the army and may have killed more than 5 million people in the Roman empire. This article published in the book was written by April Pudsey, senior lecturer in Roman History at Manchester Metropolitan University. “ Source: Disability in Antiquity,” Routledge, 2017).
-
Plague of Cyprus (AD 250-271)
It is named after St. Paul, bishop of Carthage (a city in Tunisia), who described the epidemic as a sign of the end of the world. Named after Cyprian, the Plague of Cyprus is estimated to have killed 5,000 people a day in Rome alone. In 2014, archaeologists in Luxor found what appeared to be a mass grave site of plague victims. Their bodies were covered with a thick layer of lime (lime has been used as a disinfectant throughout history). Archaeologists found three kilns used to produce lime and the remains of plague victims burned on a giant pyre.
Scientists are not sure which disease caused the epidemic. Cyprian, in his Latin work “De mortalitate”, said: “Continuous diarrhea reduced body resistance and white thrush formed in the mouth area. ” (Source: Translated by Philip Schaff from “Fathers of the Third Century: Hippolytus, Cyprian, Caius, Novatian, Appendix,” Christian Classics Ethereal Library, 1885).
-
Plague of Justinian (AD 541-542)
The Byzantine Empire was devastated by the plague of Justinian, marking the beginning of its decline. The plague resurfaced periodically thereafter. Some estimates suggest that 10% of the world’s population died.
The plague was named after Byzantine Emperor Justinian (AD 527-565). During his reign, the Byzantine Empire reached its greatest size, controlling territories stretching from the Middle East to Western Europe. Justinian built a large cathedral known as Hagia Sophia (“Holy Wisdom”) in the empire’s capital, Constantinople (modern-day Istanbul). Justinian also fell ill from the plague but survived. However, the empire gradually lost land in the period after the plague.
The Black Death, which is ranked 6th on our list of the Greatest Epidemics in History and which you often hear about; It came to Europe from Asia for the first time and left great destruction in its wake. Some estimates suggest it wiped out more than half of Europe’s population . This was caused by a strain of Yersinia pestis bacteria, probably extinct today, spread on infected rodents and by fleas. The bodies of the victims were buried in mass graves.
The plague changed the course of European history. With so many deaths, labor became harder to find, bringing better wages to workers and the end of Europe’s system of serfdom. Research shows that surviving workers had better access to meat and better quality bread.
-
Cocoliztli Epidemic (1545-1548)
The infection that caused the Cocoliztli epidemic was a viral hemorrhagic febrile illness that killed 15 million people in Mexico and Central America. Among a population already weakened by extreme drought, the disease proved to be extremely disastrous. “Cocoliztli” is an Aztec word meaning “pest”.
Analyzing DNA samples from the victims’ skeletons found that they were infected with a subspecies of Salmonella known as Salmonella Paratyphi C , which causes typhoid fever . Enteric fever can still pose a major health threat today, causing high fever, dehydration, and gastrointestinal problems.
American Plagues are a cluster of Eurasian diseases brought to the Americas by European explorers. These diseases, including smallpox, contributed to the collapse of the Inca and Aztec civilizations. Some estimates suggest that 90% of the indigenous population in the Western Hemisphere was killed.
The diseases helped a Spanish force led by Hernán Cortés conquer the Aztec capital Tenochtitlán in 1519 and another Spanish force led by Francisco Pizarro conquer the Incas in 1532. The Spanish seized territory from both empires. In both cases, the Aztec and Inca armies were devastated by disease and were unable to resist the Spanish forces. As citizens of England, France, Portugal, and the Netherlands began to explore, conquer, and settle the Western Hemisphere, they were also aided by the fact that disease greatly reduced the size of all indigenous groups opposing them.
-
The Great Plague of London (1665-1666)
It was the last major outbreak of the Black Death in Great Britain. King II It caused a very serious crisis in London, where Charles was the leader. The plague began in April 1665 and spread rapidly during the hot summer months. Fleas from plague-infected rodents were one of the main causes of transmission. By the time the plague was over, around 100,000 people had died, including 15% of London’s population. But this was not the end of that city’s suffering. On September 2, 1666, the Great Fire of London began, lasting four days and burning large parts of the city.
-
The Great Plague of Marseille (1720-1723)
Historical records say that the Great Plague of Marseille began when a cargo ship named Grand-Saint-Antoine, coming from the Eastern Mediterranean, docked in the port of Marseille, France. Although the ship was quarantined, the plague entered the city, probably via fleas on plague-infected rodents.
The plague spread rapidly, and as many as 100,000 people may have died in Marseille and the surrounding area in the three years following its arrival in port. It is estimated that 30% of Marseille’s population may have been wiped out.
-
The Greatest Epidemics in HistoryRussian Plague (1770-1772)
In plague-ravaged Moscow, the terror of quarantined citizens turned to violence. Riots spread throughout the city and resulted in the murder of Archbishop Ambrosius, who encouraged the crowds not to gather for worship.
Empress II of Russia Catherine (also called Catherine the Great) was so desperate to contain the plague and restore public order that she issued a hasty decree ordering all factories to be moved from Moscow. It is recorded that up to 100,000 people may have died from this epidemic when the plague ended.
-
Philadelphia Yellow Fever Epidemic (1793)
When yellow fever gripped the then-capital of the United States, Philadelphia, officials wrongly believed that slaves were immune. As a result, abolitionists called for the hiring of people of African descent to care for the sick.
The disease was carried and transmitted by mosquitoes, which experienced a population explosion in Philadelphia that year, especially during the hot and humid summer weather. When winter came and the mosquitoes died off, the epidemic finally stopped. By then more than 5,000 people had died.
In the modern industrial age, new transportation links facilitated the spread of influenza viruses. The disease spread around the world in just a few months, killing 1 million people. It took just five weeks for the epidemic to reach its highest death toll.
The earliest cases were reported in Russia. It spread completely to St. Petersburg before quickly spreading to the rest of Europe and the world.
-
American polio epidemic (1916)
A polio epidemic that began in New York caused 27,000 cases and 6,000 deaths in the United States. The disease mainly affected children. It could cause permanent disability or even result in death.
Polio epidemics continued to occur sporadically in the United States until the Salk vaccine was developed in 1954. As the vaccine became widely used, cases in the United States decreased. The last case of polio in the United States was reported in 1979. Worldwide vaccination efforts have greatly reduced the disease, although it has not yet been completely eliminated.
-
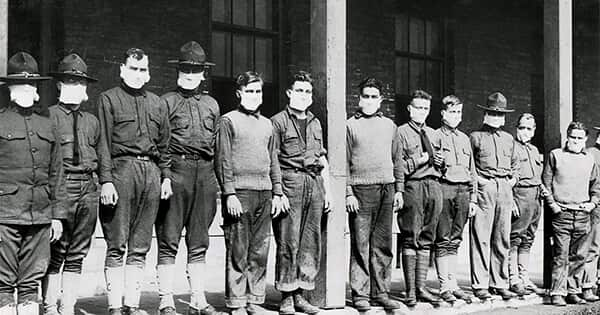
The Greatest Epidemics in History: Spanish Flu (1918-1920)
From the South Seas to the Arctic, approximately 500 million people fell victim to the Spanish Flu. One fifth of them died, and some indigenous communities were on the verge of extinction. The spread and lethality of influenza was increased by the cramped conditions of soldiers and wartime malnutrition in which many people experienced during World War I.
Despite the name Spanish Flu, the disease probably did not start in Spain. Spain was a neutral nation during the war and did not impose strict censorship on its press. He was therefore able to freely publish early records of the disease. As a result, people incorrectly believed that the disease was specific to Spain, and the name Spanish Flu was attributed to Spain.
-
Asian Flu (1957-1958)
The Asian Flu pandemic was another global case for influenza. The disease, which has its roots in China, has claimed more than 1 million lives. The virus that caused the pandemic was a mixture of bird flu viruses.
The Centers for Disease Control and Prevention noted that the disease spread rapidly and was reported in Singapore in February 1957, Hong Kong in April 1957, and coastal cities in the United States in the summer of 1957. The total number of deaths was more than 1.1 million. In the United States alone, the figure was 116,000.
-
AIDS pandemic and epidemic (1981-present)
AIDS has claimed an estimated 35 million lives since it was first diagnosed. HIV, the virus that causes AIDS, probably passed from a chimpanzee species to humans in West Africa in the 1920s. The virus spread throughout the world and AIDS became an epidemic in the late 20th century. Now, about 64% of the estimated 40 million living with human immunodeficiency virus (HIV) live in Africa.
For decades there was no known cure for the disease, but drugs developed in the 1990s now allow people with the disease to live a normal lifespan with regular treatment. Even more encouraging, two people became free of HIV as of early 2020.
-
H1N1 Swine Flu epidemic (2009-2010)
The 2009 swine flu pandemic was caused by a new H1N1 strain that emerged in Mexico in the spring of 2009 before spreading to the rest of the world. According to the CDC (Centers for Disease Control and Prevention), in one year the virus infected 1.4 billion people worldwide and killed 575,400.
The 2009 flu pandemic primarily affected children and young adults, with 80% of deaths in people under age 65, the CDC reported. This was unusual, considering that most flu viruses, including those that cause seasonal flu, cause the highest percentage of deaths in people 65 and older. But in the case of swine flu, older people appeared sufficiently immune to the group of viruses to which H1N1 belongs, so they were not as affected. A vaccine has been developed for the H1N1 virus that causes swine flu and has been incorporated into the flu vaccine.
-
West Africa Ebola outbreak (2014-2016)
Ebola devastated West Africa with 28,600 reported cases and 11,325 deaths between 2014 and 2016. The first reported case was in Guinea in December 2013. The disease then quickly spread to Liberia and Sierra Leone. Most cases and deaths occurred in these three countries. The Centers for Disease Control and Prevention reported smaller numbers of cases occurring in Nigeria, Mali, Senegal, the United States and Europe.
Although efforts to find a vaccine continue, no cure for Ebola has been found. The first known cases of Ebola occurred in Sudan and the Democratic Republic of Congo in 1976. It has been suggested that the virus may have emerged in bats.
-
Zika Virus outbreak (2015-Present)
The impact of the recent Zika outbreak in South America and Central America is unknown. Meanwhile, scientists are racing against time to control the virus. Zika virus is generally spread by Aedes mosquitoes. However, it can also be transmitted sexually in humans.
While Zika is not generally harmful to adults or children, it can attack babies still in the womb, causing birth defects. The mosquito species that carry Zika thrive best in warm, humid climates, making South America, Central America and parts of the southern United States ideal areas for the virus to thrive.
-
Covid-19 Corona Pandemic (2020 – Present)
New Coronavirus Disease (COVID-19) is a virus that was first identified on January 13, 2020, as a result of research conducted in China’s Wuhan Province in a group of patients who developed respiratory symptoms (fever, cough, shortness of breath) in late December.
The outbreak was initially detected in seafood and animal markets in this region. It was later transmitted from person to person and spread to Wuhan, other cities in the Hubei province, other provinces of the People’s Republic of China and other countries in the world.
What are the symptoms of coronavirus?
Although it has been reported that there may be asymptomatic cases, their rate is unknown. The most common symptoms are fever, cough and shortness of breath. In severe cases, pneumonia, severe respiratory failure, kidney failure and death may occur.
How is Corona Virus Transmitted?
It is transmitted by inhalation of droplets released into the environment when infected individuals cough and sneeze. The virus can also be acquired by touching surfaces contaminated with respiratory particles of patients and then touching the face, eyes, nose or mouth without washing the hands. It is risky to touch the eyes, nose or mouth with dirty hands.
Who is at More Risk with Corona Virus?
Information gained so far regarding COVID-19 infection has shown that some people are at greater risk of becoming ill and developing severe symptoms.
– 80 percent of cases have a mild disease.
– 20% of cases are treated in hospital conditions.
– The disease generally affects people aged 60 and over more.
People Most Affected by Corona Disease:
– Those over 60 years of age
– People with serious chronic medical conditions:
– Heart disease
– Hypertension
– Diabetes
– Chronic Respiratory disease
– Such as cancer
– Healthcare Workers
Are Children At Risk With Corona?
In children, the disease appears to be rare and mild.
No deaths have been observed in children so far.
Are Pregnant Women at Risk with Corona?
There is limited scientific evidence on the severity of disease in pregnant women who develop COVID-19 infection.
However, available evidence suggests that disease severity among pregnant women following COVID-19 infection is similar to non-pregnant adult COVID-19 cases, and there are no data to suggest that infection with COVID-19 during pregnancy has an adverse effect on the fetus.
There is no evidence so far that COVID-19 is transmitted from mother to baby during pregnancy.
How to Diagnose Corona Disease?
The molecular tests required for the diagnosis of New Coronavirus are available in our country. Diagnostic testing is performed only at the National Virology Reference Laboratory of the General Directorate of Public Health and designated Public Health Laboratories.
What are the Ways to Protect from Corona?
It is recommended not to travel abroad as much as possible. In cases where going abroad is mandatory, the following rules should be observed:
The basic principles recommended to reduce the general risk of transmission of acute respiratory infections also apply to the Novel Coronavirus Disease (COVID-19). These;
-Attention should be paid to hand cleaning. Hands should be washed with soap and water for at least 20 seconds, and alcohol-based hand antiseptic should be used when soap and water are not available. There is no need to use soap containing antiseptic or antibacterial, normal soap is sufficient.
– Avoid contact with mouth, nose and eyes without washing hands.
– Avoid contact with sick people (if possible, stay at least 1 m away).
– Due to the large number of patients, health centers should not be visited if possible, and in cases where it is necessary to go to a health institution, contact with other patients should be minimized.
– When coughing or sneezing, the nose and mouth should be covered with a disposable paper tissue.
– Eating raw or undercooked animal products should be avoided. Well-cooked foods should be preferred.
– Areas at high risk for general infections, such as farms, live animal markets and areas where animals may be slaughtered, should be avoided.
– If you have any respiratory symptoms within 14 days after travelling, you should wear a mask and apply to the nearest health institution, and the doctor should be informed about your travel history.